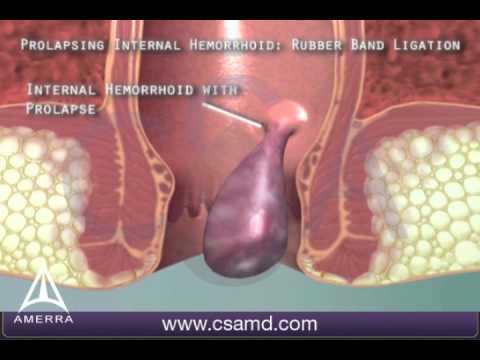
Non-Surgical Treatment of Hemorrhoids with Banding
What is Hemorrhoid Banding?
Hemorrhoid banding, also known as rubber band ligation, is a common and effective non-surgical treatment for hemorrhoids. This procedure is performed in a doctor’s office and is designed to be painless, requiring no anesthesia.
Procedure Outline
Preparation: You will be asked to lie down in a comfortable position.
Application: The doctor uses a special instrument to place a small rubber band around the base of the hemorrhoid.
Effect: The band cuts off the blood supply to the hemorrhoid, causing it to shrink and eventually fall off within a few days.
What to Expect
During the Procedure: You might feel a slight pressure or discomfort, but it should not be painful.
After the Procedure: You can go home immediately after the procedure. Some patients may experience mild discomfort or a feeling of fullness in the rectal area.
Recovery Time: Most people return to their normal activities the same day. The hemorrhoid typically falls off within 1-2 weeks.
FAQs
Q: Is the procedure painful? A: No, the procedure is designed to be painless. You may feel some pressure, but it should not be painful.
Q: Do I need anesthesia? A: No, anesthesia is not required for this procedure.
Q: How long does the procedure take? A: The procedure usually takes about 10-15 minutes.
Q: What should I do after the procedure? A: You can resume normal activities immediately. Avoid heavy lifting and straining during bowel movements.
Q: Are there any side effects? A: Some patients may experience mild discomfort, bleeding, or a feeling of fullness. These symptoms usually resolve on their own.
Q: When will the hemorrhoid fall off? A: The hemorrhoid typically falls off within 1-2 weeks after the procedure.
Q: Will I need more than one treatment? A: Some patients may require additional treatments if they have multiple hemorrhoids.
Watch Video
Hemorrhoidectomy
What is a Hemorrhoidectomy?
A hemorrhoidectomy is a surgical procedure to remove hemorrhoids, which are swollen veins in your anus that can cause pain, itching, and bleeding.
Brief Description of the Procedure
Duration: The surgery usually takes about 30 minutes to an hour.
Anesthesia: You will be given general anesthesia, so you will be asleep and won’t feel any pain during the procedure.
Process: The surgeon will remove the hemorrhoids and may use stitches to close the area.
What to Expect on the Day of Surgery
Before Surgery: You will need to fast (not eat or drink) for about 6 hours before the surgery. Your doctor may give you specific instructions about taking laxatives or enemas.
During Surgery: You will be under general or spinal anesthesia. The surgery will be performed, and you will be monitored closely.
After Surgery: You will be taken to a recovery room where you will wake up from the anesthesia. You might feel some pain and discomfort, which is normal.
Hospital Stay
Duration: Most patients can go home the same day, but some may need to stay overnight for observation.
Pain Management: You will be given pain medication to manage any discomfort.
Bleeding: Some bleeding is normal after the surgery.
FAQs
Q: How long is the recovery period? A: Recovery can take a few weeks. You may experience pain and discomfort during bowel movements, which will gradually improve.
Q: What are the risks of the surgery? A: Risks include bleeding, infection, and a temporary inability to control bowel movements. These are rare but possible.
Q: Can hemorrhoids come back after surgery? A: It’s possible for new hemorrhoids to develop, but the surgery is effective in removing the existing ones.
Q: What should I do to prepare for the surgery? A: Follow your doctor’s instructions, which may include fasting and taking specific medications.
Q: How can I manage pain after the surgery? A: Your doctor will prescribe pain medication. Sitting in warm baths and using ice packs can also help
Watch Video

Laser Surgery for Anorectal Conditions
Introduction
This leaflet provides information about laser surgery for anorectal conditions such as hemorrhoids and fistulas. It aims to help you understand the procedure, what to expect, and answer some common questions.
What is Laser Surgery for Anorectal Conditions?
Laser surgery is a minimally invasive procedure used to treat conditions like hemorrhoids and fistulas. It uses a focused beam of light (laser) to remove or shrink abnormal tissue with precision and minimal damage to surrounding areas.
Conditions Treated
Hemorrhoids: Swollen veins in the lower rectum or anus.
Anal Fistulas: Abnormal connections between the anal canal and the skin near the anus.
The Procedure
Preparation: You may be asked to fast for a few hours before the surgery. An enema might be given to clear the bowels.
Anesthesia: Local or general anesthesia will be administered to ensure you are comfortable and pain-free during the procedure.
Laser Application: The surgeon uses a laser to precisely target and treat the affected area. The laser seals blood vessels, reducing bleeding and promoting faster healing.
Completion: The procedure typically takes about 30-60 minutes. You will be monitored for a short period before being allowed to go home.
What to Expect After Surgery
Recovery: Most patients can go home the same day. You may experience mild discomfort, which can be managed with pain relief medication.
Activity: Avoid strenuous activities for a few days. Gradually return to normal activities as advised by your doctor.
Diet: Follow a high-fiber diet to prevent constipation and strain during bowel movements.
Follow-Up: Attend all follow-up appointments to ensure proper healing and address any concerns.
Frequently Asked Questions (FAQs)
Q: Is laser surgery painful? A: The procedure is performed under anesthesia, so you should not feel pain during the surgery. Post-operative discomfort is usually mild and manageable with medication.
Q: How long is the recovery period? A: Most patients recover within a few days to a week. Full recovery may take a few weeks, depending on the individual and the extent of the surgery.
Q: Are there any risks or complications? A: As with any surgery, there are risks, including infection, bleeding, and recurrence of the condition. However, laser surgery generally has a lower risk of complications compared to traditional surgery.
Q: Can I drive home after the surgery? A: It is recommended to have someone drive you home, especially if you received general anesthesia.
Q: Will I need to take time off work? A: You may need to take a few days off work to rest and recover. Your doctor will provide specific advice based on your condition and job requirements.and using ice packs can also help
Watch Video

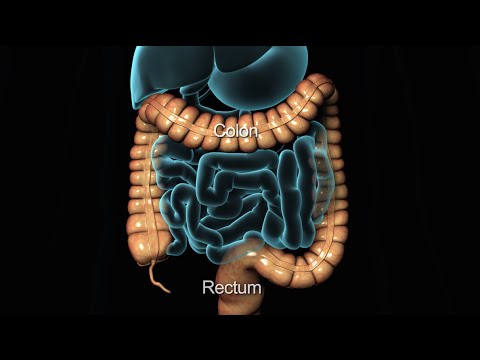
Colonoscopic Screening for Colon and Rectal Cancer
Significance of Screening
Colonoscopic screening is a crucial procedure for detecting colon and rectal cancer at an early stage. Early detection significantly increases the chances of successful treatment and can prevent the progression of cancer. Regular screenings can also identify and remove polyps before they develop into cancer.
Description of Procedure
A colonoscopy is a procedure that allows your doctor to examine the inner lining of your large intestine (colon and rectum). It is performed using a colonoscope, a long, flexible tube with a camera at the end. The colonoscope is gently inserted through the rectum and advanced through the colon. The camera transmits images to a monitor, allowing the doctor to inspect the colon for abnormalities.
What to Expect
Preparation:
You will need to follow a special diet and take a bowel-cleansing solution the day before the procedure to ensure your colon is empty.
You may need to stop certain medications temporarily.
During the Procedure:
You will be given a sedative to help you relax and minimize discomfort.
The procedure typically takes about 30 to 60 minutes.
You may feel mild cramping or pressure as the colonoscope is moved through your colon.
After the Procedure:
You will be monitored until the sedative wears off.
You may experience some bloating or gas, which should resolve quickly.
You will need someone to drive you home due to the sedative effects.
Frequently Asked Questions (FAQs)
Q: How often should I have a colonoscopy? A: It is generally recommended to have a colonoscopy every 10 years starting at age 50, or earlier if you have a family history of colon cancer or other risk factors.
Q: Is the procedure painful? A: Most patients experience minimal discomfort due to the sedative. You may feel some pressure or cramping, but it is usually well-tolerated.
Q: What are the risks of a colonoscopy? A: While complications are rare, they can include bleeding, perforation of the colon, or adverse reactions to the sedative. Your doctor will discuss these risks with you before the procedure.
Q: Can I eat normally after the procedure? A: Yes, you can usually resume your normal diet after the procedure, but it’s best to start with light meals and avoid heavy or greasy foods initially.
Q: What if a polyp is found? A: If a polyp is found, it can often be removed during the colonoscopy. The polyp will be sent to a lab for analysis to determine if it is benign or cancerous.
Watch Video
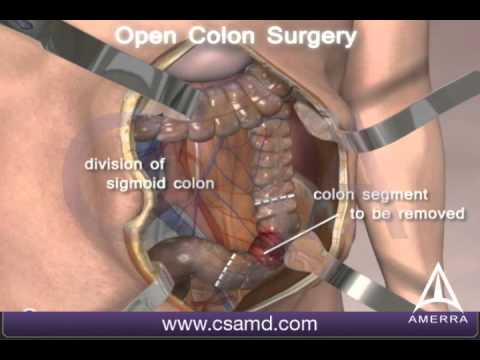
Surgery for Colorectal Cancer
Introduction
This leaflet provides essential information about colorectal cancer surgery, including the procedures, what to expect, hospital stay duration, and answers to common questions.
Description of Procedures
Polypectomy and Local Excision:
Polypectomy: Removal of polyps during a colonoscopy using a wire loop.
Local Excision: Removal of small cancers and some surrounding tissue through a colonoscope1.
Colectomy:
Partial Colectomy: Removal of the cancerous part of the colon and some surrounding healthy tissue. The remaining sections are reattached1.
Total Colectomy: Removal of the entire colon, usually only if there are other issues like multiple polyps or inflammatory bowel disease1.
Laparoscopic Surgery:
Patient Expectations
Pre-Surgery: You may need to follow a special diet and use laxatives to empty your colon.
During Surgery: The procedure will be performed under general anesthesia.
Post-Surgery: You may experience some pain and will be given medication to manage it. You will also be encouraged to move around to aid recovery.
Length of Stay in Hospital
Polypectomy and Local Excision: Usually outpatient procedures; you can go home the same day.
Partial Colectomy: Typically requires a hospital stay of 3-7 days.
Total Colectomy: Hospital stay may be longer, depending on recovery and any complications1.
General Information
Diet: You may need to follow a specific diet post-surgery to aid recovery.
Activity: Gradual return to normal activities is encouraged, but avoid heavy lifting for a few weeks.
Follow-Up: Regular follow-up appointments will be scheduled to monitor your recovery and check for any signs of recurrence.
FAQs
Will I need a stoma?
In some cases, a temporary or permanent stoma may be necessary. Your surgeon will discuss this with you before the operation.
What are the risks of surgery?
Risks include infection, bleeding, and complications related to anesthesia. Your surgical team will take steps to minimize these risks.
How long will it take to recover?
Recovery time varies, but most patients can return to normal activities within a few weeks to a few months.
Will I need additional treatment?
Depending on the stage of cancer, you may need chemotherapy or radiation therapy after surgery.
Watch Video
Keyhole (Laparoscopic) Surgery
Introduction
Keyhole surgery, also known as laparoscopic surgery, is a minimally invasive procedure used to treat various conditions. This leaflet provides information on keyhole surgery for the gall bladder, hernia, and appendix.
Gall Bladder Surgery (Cholecystectomy)
Description:
Purpose: To remove the gall bladder, usually due to gallstones causing pain or infection.
Procedure: Small incisions are made in the abdomen. A laparoscope (a thin tube with a camera) and surgical instruments are inserted to remove the gall bladder.
Patient Expectations:
Before Surgery: You may need to fast and avoid certain medications.
During Surgery: Performed under general anesthesia, typically lasting 1-2 hours.
After Surgery: Expect some pain and discomfort. Most patients go home the same day or the next.
FAQs:
How long is the recovery?
Most people return to normal activities within a week.
Are there dietary restrictions post-surgery?
Initially, a low-fat diet is recommended.
What are the risks?
Risks include infection, bleeding, and injury to nearby organs.
Hernia Repair
Description:
Purpose: To repair a hernia, which is a bulge of an organ or tissue through an abnormal opening.
Procedure: Small incisions are made, and a laparoscope and instruments are used to push the herniated tissue back and reinforce the area with mesh.
Patient Expectations:
Before Surgery: You may need to fast and avoid certain medications.
During Surgery: Performed under general anesthesia, typically lasting 1-2 hours.
After Surgery: Expect some pain and discomfort. Most patients go home the same day.
FAQs:
How long is the recovery?
Most people return to normal activities within 1-2 weeks.
Will the hernia come back?
Recurrence is rare but possible.
What are the risks?
Risks include infection, bleeding, and injury to nearby organs.
Appendix Surgery (Appendectomy)
Description:
Purpose: To remove the appendix, usually due to appendicitis (inflammation of the appendix).
Procedure: Small incisions are made, and a laparoscope and instruments are used to remove the appendix.
Patient Expectations:
Before Surgery: You may need to fast and avoid certain medications.
During Surgery: Performed under general anesthesia, typically lasting 1-2 hours.
After Surgery: Expect some pain and discomfort. Most patients go home the same day or the next.
FAQs:
How long is the recovery?
Most people return to normal activities within 1-2 weeks.
Are there any long-term effects?
No significant long-term effects are expected.
What are the risks?
Risks include infection, bleeding, and injury to nearby organs.
General Tips for Recovery
Follow your doctor’s instructions: Take prescribed medications and attend follow-up appointments.
Rest and gradually increase activity: Avoid strenuous activities until your doctor advises.
Watch for signs of complications: Contact your doctor if you experience severe pain, fever, or unusual symptoms.
Watch Video







